In the quest for effective scar treatment, researchers have turned their attention towards the promising potential of collagen. Burns, whether minor or severe, can leave behind unsightly scars that not only serve as a reminder of trauma but can also significantly impact a person’s self-esteem and quality of life.
Thus, understanding the correlation between collagen and scar appearance is crucial in developing innovative strategies to minimize their visibility and promote optimal skin regeneration.
This article explores the current scientific knowledge surrounding the effect of collagen on scar appearance after burns and sheds light on the potential of this protein as a therapeutic agent in scar management.
Click Here if You Prefer to Listen to Quick Summary Content of the Blog Post about The Collagen and Skin Scar.
The Role of Collagen in Wound Healing
Overview of wound healing process
Wound healing is a complex physiological process that involves a series of events aimed at repairing damaged tissues and restoring their integrity. It can be divided into three main stages: inflammation, tissue formation, and remodeling.
The process begins with the body’s response to injury, which triggers inflammation to control bleeding and prevent infection. Following this, the body initiates tissue formation by synthesizing and depositing collagen, the main structural protein in the extracellular matrix.
Finally, the wound undergoes remodeling, where the newly formed collagen fibers are reorganized to increase tensile strength and improve overall tissue function.
Collagen synthesis and deposition in wound healing
Collagen plays a pivotal role in wound healing, particularly in the tissue formation stage. Synthesized by fibroblasts, collagen is secreted into the wound bed, providing structural support and promoting cellular migration and proliferation.
As the wound progresses through the healing process, the deposition of collagen increases, leading to the formation of a scar. The composition of collagen in scar tissue differs from that of normal tissue, resulting in distinct physical and functional properties.
Understanding the intricacies of collagen synthesis and deposition is crucial in comprehending the subsequent effects on scar formation and appearance.
Scar Formation After Burns
Classification of burn injuries
Burn injuries are classified based on the severity and depth of tissue damage. The most commonly used classification system is the degree of burns: first-degree, second-degree, and third-degree.
First-degree burns affect only the outermost layer of the skin, while second-degree burns extend into the underlying layers.
Third-degree burns are the most severe, involving the entire thickness of the skin and potentially affecting underlying structures such as muscles and bones. The extent and depth of the burn injury significantly impact the subsequent wound healing process and scar formation.
Phases of burn wound healing
The wound healing process following a burn injury can be categorized into three main phases: the inflammatory phase, the proliferative phase, and the remodeling phase. In the inflammatory phase, damaged tissues release inflammatory mediators, initiating the body’s immune response and preparing the wound bed for repair.
The proliferative phase is characterized by collagen synthesis and deposition, angiogenesis, and re-epithelialization. Finally, in the remodeling phase, the scar undergoes changes in collagen organization and composition, leading to scar maturation and the potential for scar revision treatments.
Collagen Composition in Scar Tissue
Differences between normal and scar collagen
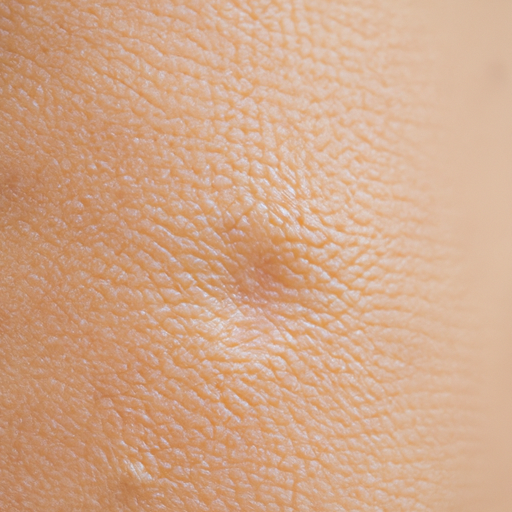
The collagen found in scar tissue differs from that of normal tissue in several key aspects. Scar collagen fibers are often disorganized and less dense compared to the well-organized and densely-packed collagen fibers in healthy tissue. This lack of organization contributes to the visible texture and raised appearance of scars.
Additionally, scar collagen may have a different composition, with altered ratios of collagen types I and III. Collagen type III is initially present in abundance during the early stages of wound healing but gradually gets replaced by collagen type I, which provides greater tensile strength. These differences in collagen composition contribute to the unique characteristics and appearance of scars.
Effect of collagen on scar appearance
Collagen plays a significant role in determining the appearance of scars. The amount and organization of collagen directly influence the texture, color, and overall quality of the scar. Excessive collagen production can lead to hypertrophic scars or keloids, which are characterized by raised, thickened, and discolored tissue.
On the other hand, insufficient collagen production may result in atrophic scars, which are characterized by depressed and sunken areas. Achieving a balanced and properly organized collagen network is essential for minimizing scar visibility and maximizing aesthetic outcomes.

Factors Influencing Collagen Production
Aging
Collagen production naturally declines with age, contributing to the increased prevalence of scars and delayed wound healing in older individuals. Aging affects the function of fibroblasts, the cells responsible for collagen synthesis, leading to reduced collagen production and impaired wound healing.
Furthermore, the quality of collagen fibers also deteriorates with age, resulting in weaker and less elastic scar tissue. Understanding how age-related changes influence collagen production can guide the development of interventions targeting scar management in the elderly population.
Genetics
Genetics can influence collagen production and affect the healing process. Variations in genes involved in collagen synthesis and remodeling pathways can impact the quantity and quality of collagen produced.
Genetic factors can contribute to certain individuals being more prone to excessive scarring or poor wound healing. Identifying specific genetic markers associated with collagen production can provide insights into personalized approaches to scar management and potentially guide the development of targeted interventions.
Nutrition and diet
A balanced diet rich in essential nutrients is crucial for optimal collagen synthesis and wound healing. Nutrients such as vitamin C, zinc, and copper play key roles in collagen production, while deficiencies in these nutrients can impair the synthesis and deposition of collagen in the wound bed.
Consuming a diet abundant in fruits, vegetables, and lean proteins can supply the necessary building blocks for collagen production, promoting effective wound healing and minimizing scar formation.
Infections and inflammation
Infections and chronic inflammation can disrupt the normal wound healing process and negatively impact collagen production. Inflammatory mediators released during the initial stages of wound healing help orchestrate the synthesis and deposition of collagen. However, persistent or excessive inflammation can result in abnormal collagen production and impaired scar formation.
Additionally, infections can introduce bacteria that directly degrade collagen and hinder the healing process. Effective infection control measures and appropriate management of inflammation are crucial in optimizing collagen production and scar outcomes.
External treatments and interventions
Various external treatments and interventions have been developed to influence collagen production and improve scar appearance. Techniques such as laser therapy, microneedling, and radiofrequency can stimulate collagen synthesis and remodeling, promoting scar reduction.
Additionally, the use of topical products containing collagen or collagen-derived peptides can provide external sources of collagen to supplement or enhance the body’s natural production.
Understanding the impact of these interventions on collagen synthesis and their potential in scar management is essential for providing evidence-based and effective treatment strategies.
Role of Collagen in Scar Maturation
Wound contraction
Collagen plays a crucial role in wound contraction, a process that occurs during the proliferative phase of wound healing. Myofibroblasts, specialized cells involved in wound contraction, interact with collagen fibers and exert mechanical forces to pull the wound edges closer together.
Collagen acts as the scaffold for myofibroblast attachment and contraction, facilitating wound closure and minimizing scar size. The proper organization and alignment of collagen fibers are essential for the effective transmission of forces and optimal wound contraction.
Scar remodeling and maturation
Following wound closure, the scar continues to undergo remodeling and maturation. This process involves further reorganization of collagen fibers and a gradual increase in tensile strength. Over time, the scar becomes less visible and blends in better with the surrounding skin.
Collagen turnover and remodeling help refine the scar’s appearance and improve its functionality. By understanding the underlying mechanisms of scar remodeling and maturation, interventions can be developed to optimize this process and achieve better scar outcomes.
Clinical Studies on Collagen’s Effect on Scar Appearance
Methodology and design of relevant studies
Numerous clinical studies have explored the effect of collagen on scar appearance. These studies employ various methodologies, including objective assessments such as scar thickness measurements, scar color analysis, and patient-reported outcome measures.
Randomized controlled trials are often considered the gold standard in evaluating the effectiveness of collagen-based interventions. These studies utilize control groups receiving a placebo or alternative treatment to compare the outcomes of collagen-treated individuals.
The design and execution of these studies are crucial in obtaining reliable and meaningful results.
Analysis of scar appearance and collagen levels
In clinical studies, scar appearance is assessed using standardized scales and scoring systems. Objective measurements such as scar color, texture, and pliability are often recorded, while patient-reported outcomes provide valuable insights into the perceived aesthetic outcomes.
Collagen levels within scar tissue can also be analyzed using various techniques, including immunohistochemistry and biochemical assays. Correlating collagen levels with scar appearance parameters can help establish a link between collagen production and scar outcomes.
Comparison between control and collagen-treated groups
Clinical studies often compare the outcomes of control groups with those receiving collagen-based interventions. These comparisons help determine the effectiveness of collagen treatments in improving scar appearance.
Collagen-based interventions may include topical applications, injectable fillers, or the use of collagen dressings and scaffolds. Evaluating parameters such as scar size, color, texture, and patient satisfaction allows for an objective assessment of the benefits of collagen-based interventions.
Well-designed and carefully executed studies are vital in providing robust evidence to guide clinical decision-making.

Effectiveness of Collagen-based Interventions
Topical application of collagen-based products
Topical application of collagen-based products, such as creams and gels, is a common approach in scar management. Collagen, when applied topically, can directly stimulate fibroblasts’ activity and enhance collagen synthesis in the wound bed.
These interventions aim to improve scar appearance by promoting the deposition of well-organized collagen fibers and reducing scar thickness. Clinical studies have shown promising results, with improvements observed in scar texture, pliability, and overall aesthetic outcomes.
However, the effectiveness of topical collagen treatments may vary depending on individual factors, such as the type and severity of the scar.
Injectable collagen fillers
Injectable collagen fillers have gained popularity in scar management, especially for atrophic or depressed scars. By injecting collagen directly into the scar, volume and support are restored, resulting in a smoother and more elevated scar surface.
Collagen fillers can temporarily improve the appearance of scars, providing immediate aesthetic benefits. However, the effects are not permanent, and repeated treatments may be necessary.
Additionally, the use of injectable collagen fillers carries associated risks, such as allergic reactions and infections, which should be carefully considered before undergoing treatment.
Collagen dressings and scaffolds
Collagen-based dressings and scaffolds have been developed to provide a three-dimensional framework for wound healing and facilitate the deposition of new collagen.
These products can enhance the body’s natural healing processes, promote cell migration, and provide a moist environment conducive to optimal collagen synthesis. Collagen dressings and scaffolds have shown promise in improving scar outcomes, particularly in chronic wounds and complex surgical incisions.
However, the efficacy of these interventions may be influenced by factors such as wound characteristics and individual patient factors. Further research is needed to optimize their use and establish standardized protocols for their application.
Potential Side Effects and Risks of Collagen Treatment
Allergic reactions
Collagen-based interventions, particularly those derived from bovine or porcine sources, carry a risk of allergic reactions. Some individuals may develop hypersensitivity to collagen, leading to localized or systemic allergic responses.
Symptoms can range from mild itching and redness to severe anaphylaxis, a life-threatening allergic reaction. Pre-treatment allergy testing is recommended to identify individuals at risk and prevent adverse reactions.
Alternative collagen sources, such as synthetic or human-derived collagen, may be considered to minimize the risk of allergic responses.
Infections
Invasive collagen-based interventions, such as injectable fillers or surgical incorporation of collagen implants, carry a risk of infection. Bacterial contamination during the procedure can lead to localized or systemic infections, adversely affecting wound healing and scar outcomes.
Proper disinfection and sterilization techniques, along with strict adherence to aseptic protocols, are essential in minimizing infection risks. Prompt identification and management of infections are crucial for favorable scar healing and overall patient well-being.
Granulomas and nodule formation
Collagen treatments, particularly injectable fillers, can occasionally lead to the formation of granulomas or nodules. Granulomas are inflammatory reactions characterized by the formation of localized nodules.
They can arise as a result of the body’s immune response to the presence of foreign substances, such as collagen. Granulomas can be aesthetically displeasing and may require additional interventions, such as steroid injections or surgical excision.
Careful patient selection, proper injection techniques, and vigilant monitoring can help minimize the risk of granuloma formation.

Combination Therapies for Scar Management
Collagen combined with other wound healing agents
Combining collagen-based interventions with other wound healing agents and modalities can maximize scar management outcomes. Adjunctive therapies, such as silicone sheets or gels, have been shown to enhance the effectiveness of collagen treatments.
Silicone helps create a favorable environment for collagen synthesis and remodeling, optimizing scar texture and color. Furthermore, combining collagen treatments with other modalities, such as laser therapy or microneedling, can stimulate collagen production and further improve scar appearance.
Personalized treatment plans that integrate multiple interventions tailored to individual patient needs can provide comprehensive and superior scar management.
Collagen in conjunction with laser therapy
Laser therapy, when used in conjunction with collagen-based interventions, can significantly improve scar appearance. Laser technology can selectively target scar tissue, stimulating collagen production and remodeling to reduce scar size, redness, and texture irregularities.
The thermal effect of lasers also promotes vascularization, enhancing wound healing and scar maturation. Combining collagen treatments with laser therapy allows for synergistic effects, providing comprehensive scar improvement.
However, proper patient selection, adherence to laser safety protocols, and skilled administration are crucial in maximizing the benefits and avoiding potential complications.
Combination of collagen and silicone sheets/gels
The use of collagen treatments in combination with silicone sheets or gels has shown promise in scar management. Silicone products create a protective barrier over the scar, maintaining an optimal moisture balance and reducing scar visibility.
When used in conjunction with collagen-based interventions, silicone sheets or gels enhance collagen synthesis and promote scar remodeling. This combination approach can lead to improved scar texture, pliability, and overall aesthetic outcomes.
Personalized treatment plans that leverage the benefits of both collagen and silicone products can offer superior scar management results.
Future Perspectives and Conclusion
Advancements in collagen-based interventions hold tremendous potential in scar management. Continued research efforts aimed at understanding collagen synthesis, deposition, and remodeling will contribute to the development of more effective treatment strategies.
Further optimization of collagen-based interventions, such as the use of novel delivery systems and combination therapies, may improve overall scar outcomes.
Personalized approaches, guided by individual factors such as age, genetics, and wound characteristics, will likely shape the future of scar management. By harnessing the power of collagen and combining it with advanced interventions, the goal of minimizing scar appearance and maximizing aesthetic outcomes can be achieved.
Further research, collaboration, and optimization are required to unlock the full potential of collagen in scar management and provide patients with the best possible care. In summary, collagen plays a crucial role in wound healing and scar formation, and its impact on scar appearance is significant.
Understanding the factors influencing collagen production and the effectiveness of collagen-based interventions allows for tailored and evidence-based scar management strategies.
With advancements in technology and a deeper understanding of collagen’s role, the future of scar management holds great promise.